 Introduction
Introduction
Injuries can be deliberate or unintentional and are one of the top ten leading causes of death and disability worldwide. Unspecified falls, which most people call “trivial falls,” have been identified as the second leading cause of disability and illness, especially among older people.
On the one hand, more people are breaking their hips, and on the other, people are living longer. This has pushed orthopedic surgeons to develop better ways to fix broken hips so that older people don’t get stuck in a cycle of immobility, bedsores, septicemia, and death.
Understanding Proximal Femoral Nail Antirotation (PFNA)
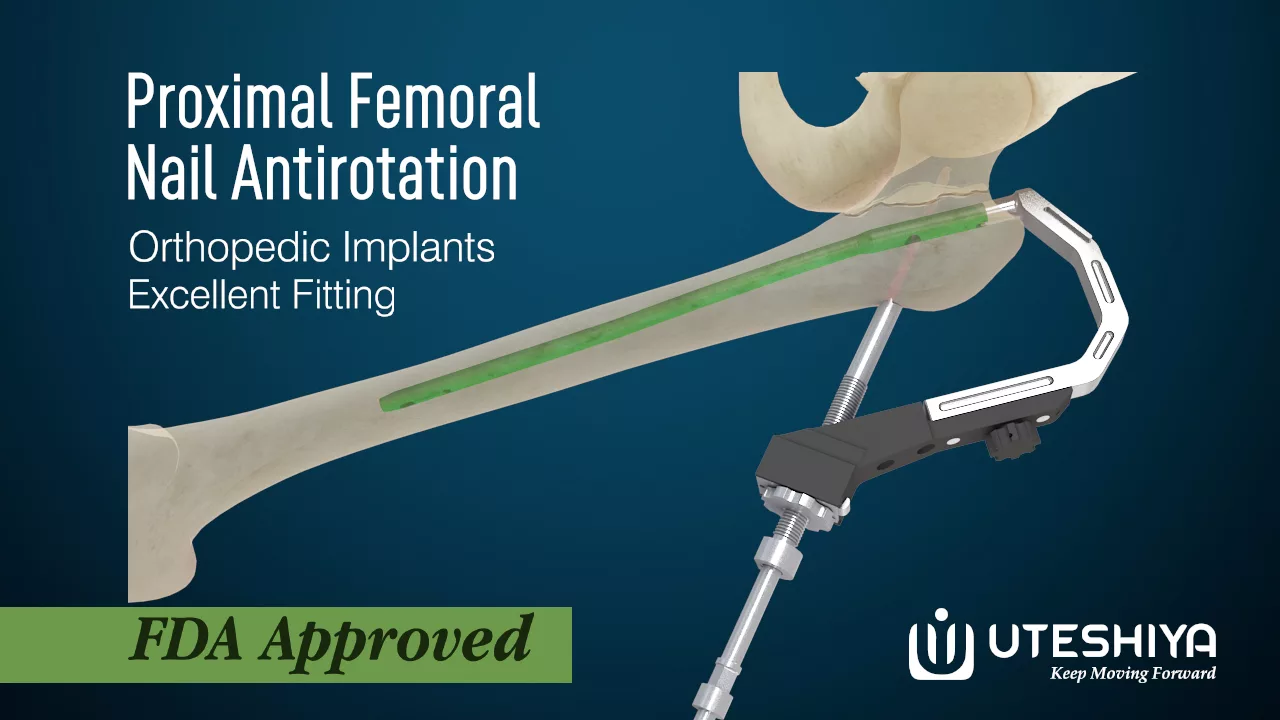
The Proximal Femoral Nail Antirotation (PFNA) is a medical implant used to treat proximal femur fractures, especially in older people with osteoporosis. It’s made to provide steady fixation and encourage early movement.
The PFNA comprises a long intramedullary nail that is put through a small cut into the femoral canal. The tip of the nail is a spiral blade put in the femoral head to stop the nail from turning. It is named antirotation because the proximal end of the nail has a locking device that keeps it from turning.
The Proximal Femoral Nail Antirotation lets the nail and the bone around it share the load. It helps the fracture heal and lowers the chance that the implant will fail.
Indications for PFNA
Proximal Femoral Nail Antirotation works well in following medical conditions.
-> Intertrochanteric fractures: PFNA often repairs femur fractures between the greater and lesser trochanters. It stabilizes and mobilizes these fractures.
-> Subtrochanteric fractures: PFNA can be utilized for fractures below the intertrochanteric zone but above the femoral shaft. The implant’s antirotation feature stabilizes and heals the fracture.
-> Reverse oblique fractures: PFNA works well on femur fractures that angle from the lateral to the medial side. PFNA’s helical blade shape improves fracture anchoring and stability.
-> Osteoporotic fractures: Because elderly people with osteoporosis have weaker bones, PFNA is often recommended. Stabilizing osteoporotic bone fractures with the implant’s load-sharing and rotational stability.
-> Unstable fractures: When sliding hip screws don’t work, PFNA may. In difficult fracture patterns, PFNA’s antirotation mechanism prevents implant cut-out or collapse, lowering implant failure.
PFNA surgical technique: Step-by-step procedure
PFNA surgical technique: Step-by-step procedure involves the following method
1. Positioning: The patient lies supine on a fracture table with the injured leg wrapped.
2. Incision and exposure: A tiny incision is made over the lateral proximal femur. The greater trochanter and nail entrance site are exposed by gently dissecting soft tissues.
3. Nail insertion: Fluoroscopically guided nail insertion into the femoral canal. After positioning the guide wire, a cannulated drill prepares the femoral canal.
4. Nail placement: The guide wire puts the pre-measured PFNA nail into the femoral canal. Fluoroscopy confirms nail location.
5. Blade insertion: Insert the nail’s helical blade into the femoral head. To achieve rotational stability, location and insertion depth are carefully considered.
6. Proximal locking: Locking screws or nuts secure the nail’s proximal end. These screws stabilize the nail by engaging the bone.
7. Wound closure: After the wound has been cleaned and sterilized, it is closed in layers to prevent excessive bleeding. Sterile dressings cover the wound.
Potential Complications and Risk Mitigation
PFNA may cause:
-> Infection: Sterility and preventive medications reduce infection risk.
-> Implant malposition: Preoperative planning, intraoperative imaging, and careful surgery can reduce implant malposition.
-> Intraoperative fractures: Gentle nail insertion and treatment of fracture fragments can prevent subsequent fractures.
-> Implant failure: Proper fracture reduction, implant sizing, and patient selection reduce implant failure.
-> Leg length discrepancy: Preoperative assessments and intraoperative methods can reduce the risk.
Clinical Outcomes and Evidence
Clinical results and data show that Proximal Femoral Nail Antirotation (PFNA) can effectively treat proximal femur fractures. Fracture healing, functional outcomes, and patient satisfaction have all been demonstrated to improve across a wide range of research.
The results of these trials show that PFNA is a promising technique for achieving stable fixation, facilitating early mobilization, and lowering the probability of implant-related problems. Clinical results and complication rates for some types of fractures treated with PFNA have improved compared to those treated with alternative fixing procedures.
Long-term tests have also shown that PFNA implants are strong and long-lasting.
Rehabilitation and Recovery
After PFNA surgery, rehabilitation is essential for a full recovery. The goals of the rehabilitation program are to improve functional results, speed up bone regeneration, and forestall problems.
Soon after surgery, patients are often instructed to begin early mobilization, weight-bearing if tolerated, and range-of-motion exercises.
To help patients return to their pre-fracture level of function, physical therapists use a variety of techniques like
-> Strengthening exercises
-> Gait training
-> Balance exercises
-> Functional activities
The patient’s condition, the type of fracture, and the surgeon’s recommendations all play a role in determining the length and rigor of the rehabilitation program. The purpose of rehabilitation is to speed up the healing process, boost morale, and make it easier to return to regular life.
Case Studies and Patient Stories
Real-life accounts from patients who have undergone PFNA surgery provide invaluable insight. These stories give first-hand reports of how the surgery affected their fracture healing, pain relief, mobility, and quality of life in general.
In their stories, patients often talk about the difficulties they faced during the recovery process, the goals they reached, and the good results they got from PFNA.
These stories can help patients understand the possible benefits and risks of the operation. They can also reassure and encourage people to consider getting PFNA surgery.
Also, case studies add to the existing body of clinical evidence by presenting unusual or difficult cases, sharing surgical methods, and discussing specific patient outcomes.
Advances and Innovations in PFNA
Proximal Femoral Nail Antirotation (PFNA) focuses on improving surgical methods and implant design. One area of progress is the development of minimally invasive techniques, which allow for smaller cuts and less damage to the soft tissues.
Nail insertion innovations, such as specialized devices and guides, aim to improve precision and prevent intraoperative problems. The helical blade and locking mechanisms have been modified to improve rotational stability and load-sharing.
These ongoing improvements aim to improve the way surgery is done, how well implants work, and how quickly patients heal from PFNA procedures.

