 Orthopedic surgery frequently uses prosthetic implants to substitute for damaged or affected joints, with hip and knee replacements being prevalent treatments. Modular cemented stems have been increasingly important in these procedures in recent years. The next section will provide a comprehensive discussion of the basic concepts, constituent elements, benefits, and surgical techniques related to modular cemented stems in orthopedic surgery.
Orthopedic surgery frequently uses prosthetic implants to substitute for damaged or affected joints, with hip and knee replacements being prevalent treatments. Modular cemented stems have been increasingly important in these procedures in recent years. The next section will provide a comprehensive discussion of the basic concepts, constituent elements, benefits, and surgical techniques related to modular cemented stems in orthopedic surgery.
What is Cemented Stems
Cemented stems are components of joint replacements that are placed into the medullary canal of the bone. Usually, they are constructed using biocompatible substances, such as metals or ceramics. Cement is frequently employed to anchor the implant, ensuring stability and promoting a process called Modular cemented stems, which offer more flexibility and adaptability in joint replacement treatments.
Components of Modular Cemented Stems
Modular cemented stems used in orthopedic surgery comprise many important parts that form the implant. Mixing and matching these parts according to the patient’s anatomy and their individual surgical needs is
essential.
In order to create a secure and functioning joint replacement, surgeons take into consideration while choosing and combining these components like,
- The patient’s anatomy
- Activity level
- General Health
Modular cemented stems usually consist of the following essential components:
1. Stem
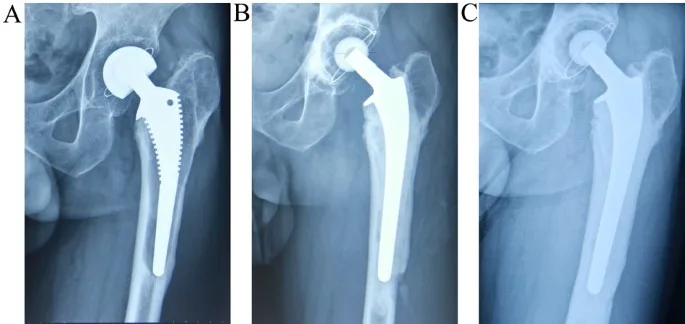
The stem is the primary implant component that enters the bone through the medullary canal. It helps keep the prosthesis in place and gives it support. A wide range of sizes and forms of stems are available to suit a variety of patient anatomy.
2. Neck
The neck is an intermediate component between the stem and the head of the implant.
How long the prosthesis is and how stable it is are both affected by it. Various neck lengths may be offered to provide correct biomechanics and accommodate different patient anatomy.
3. Head
The articulating surface of an implant is located on the topmost portion, the head. Materials and sizes can vary; a few scenarios are metal, ceramic, and highly cross-linked polyethylene. The durability and functionality of an implant are affected by the material used for the head.
4. Modular Junctions
These interfaces connect the stem, neck, and head parts. These connectors make the system modular, so surgeons can change parts as needed during implantation. Individual patient demands can be better met through modular design’s flexibility and personalization.
5. Fixation with Cement
It is common practice to use cement to anchor the implant to the bone’s medullary canal. A cement fixation system aids in the implant’s integration with the bone and offers instant stability. Surgical preferences and patient considerations might influence the cement type and method choice.
6. Collar
Modular cemented stems come with an extension that goes around the top of the stem. By stabilizing the implant, the collar reduces the
possibility of collapse, which occurs when the implant sinks into the bone. Potentially, it contributes to the transmission of stress and the distribution of loads.
7. Taper Design
The geometry of the connections between modular components is known as the taper design. The connection strength and stability are affected by the taper design. Reducing the possibility of fretting, corrosion, and other issues at the modular joints depends on a well-designed taper.
8. Bearing surface
The bearing surface is the part of the joint where the head meets the corresponding surface of the socket component. In terms of wear rates and long-term performance, the choice of bearing surface material is significant.
Advantages of Modular Cemented Stems
When it comes to joint replacement treatments, modular cemented stems are the way to go because of all the benefits they provide in orthopedic surgery.
All things considered, these benefits add to the success and adaptability of modular cemented stems in meeting the varied requirements of patients.
- The flexible design lets you make changes that make the device fit each patient’s body better.
- Surgeons have the freedom to select from a variety of stem diameters, neck lengths, and head choices, helping them to meet the specific needs of their patients.
- By enabling the replacement of individual components rather than the complete implant, modular components make revision procedures easier.
- Because modular stems may be adjusted to different scenarios, hospitals don’t require an extensive range of implant sizes, so they can keep a lower inventory.
Step of surgical procedure
The surgical procedure for implanting modular cemented stems in orthopedic surgery involves several key steps.
Any particular processes involved in the surgery could change depending on the extent to which surgical methods, implant designs, and materials have come.
Surgeons may adopt minimally invasive procedures or use computer-assisted navigation for more accuracy and faster healing. Variations in anatomy and patient-specific factors also significantly impact the tailoring of the surgical strategy.
In order to give their patients the best care possible after joint replacement procedures, surgeons need to keep up with the newest research in the area.
Step of surgical procedure of Modular Cemented Stems
- Planning Before the Operation
- How to Position the Patient
- Opening for Surgery
- A Dissection of the Soft Tissues
- Preparation of the Bones for Joint Exposure
- Attempts at Implantation
- The Application of Cement
- Positioning of Components
- The process of closing the incision
Challenges and Limitations
- Anxieties and Deterioration
The connections between the various parts of a modular cemented stem are prone to fretting and corrosion. The continuous discharge of wear particles into the surrounding tissues may cause irritation or damage over time.
Surgeons should look into the consequences for patient outcomes as they pertain to the meticulous monitoring of fretting and corrosion’s long-term impacts.
- Risk of infection
While the modular design may provide some flexibility, it also creates more voids around the components, which might be a breeding ground for germs. Infection, a significant problem that can cause implant failure, is more likely due to this more substantial surface area.
Medical professionals must adhere to stringent infection prevention protocols to lessen the likelihood of infection before, during, and after surgery.
- Prevention of stress
Cemented stems carry the risk of stress shielding, a condition in which the body’s average ability to transmit stress to bones is impaired.
Because of this, bone may resorb around the implant, which might affect the joint replacement’s stability in the long run. Surgical planners must carefully weigh the advantages of cemented fixation against the risks of stress shielding.
- Complications associated with reconstruction surgery
Re-surgeries can still be complicated, even with modular components that make them easier than non-modular implants. Addressing modular connections adds a level of complexity to revision procedures that may be required owing to wear, loosening, or other issues. The difficulties of revision surgeries require surgeons to be experienced and knowledgeable.
Wrapping It Up
Modular cemented stems have transformed joint replacement operations in orthopedic surgery by allowing for personalization, flexibility, and adaptation to each patient’s unique requirements. Optimal patient care and adequate joint replacements depend on a thorough understanding of modular cemented stems, which is becoming more important in orthopedic surgery.

