 Introduction
Introduction
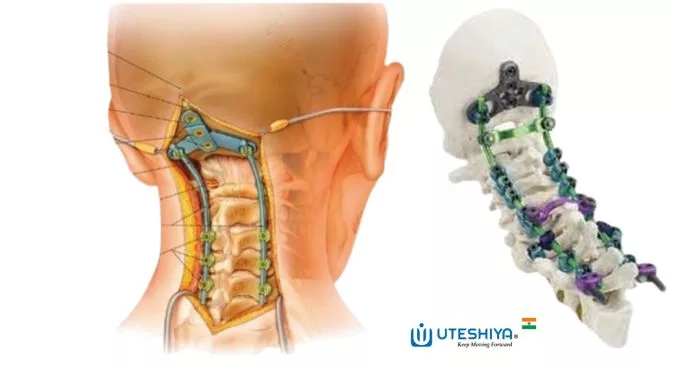
Occipitocervical Fusion System: The spine is a phenomenal structure that gives us support and movement. The occipitocervical region, which connects the brain to the upper cervical vertebrae and is a key part of how the head moves and stays stable, is one of its most essential parts.
Over the years, occipitocervical fusion has become an essential surgical technique for treating a number of conditions that affect this area.
The research and development of occipitocervical systems have made incredible progress, leading to significant breakthroughs that have changed how patients are cared for and their outcomes.
Understanding Occipitocervical Fusion
Occipitocervical fusion is a surgical treatment in which the occipital bone is permanently fixed to the upper cervical vertebrae.
This procedure is often used to handle traumatic injuries, birth defects, tumors, and diseases that cause the occipitocervical junction to break down. By strengthening this area, occipitocervical fusion stops this area from moving too much, reduces pain, and helps prevent nerve problems.
Evolution of Occipitocervical Systems
In the past, occipitocervical fusion was done with wiring and bone grafting, but the outcomes were often in doubt, and there was a high risk of the bones not joining or the hardware failing. But changes in medical technology and surgery have changed the field of occipitocervical systems.
In the last few decades, surgeons have been able to do more accurate and stable fusions using advanced tools like occipitalcervical plates, cervical screws, rods, and interbody spacers.
These improvements have greatly reduced the chance of complications, increased the number of successful fusions, and helped patients have better outcomes.
Benefits and Features of Modern Occipitocervical Systems
The modern occipitocervical fusion systems offer many advantages over previous versions, including the following
Improved Stability
Modern instruments provide tight fixation, which makes fusion work better and lowers the risk of implant-related problems.
Personalized Approach
Customizable options enable surgeons to adapt the system to each patient’s unique anatomy, leading to more successful outcomes of the occipitocervical fusion system.
Minimally Invasive Techniques
Less invasive treatments mean less pain after surgery, quicker recovery, and a better patient experience.
Advanced Imaging and guidance
When combined with advanced imaging technologies and guidance systems, it is possible to place implants more precisely, making surgery more accurate.
Biocompatible Materials
Biocompatible materials reduce the risk of bad effects and improve how well an implant works over time.
Case Studies and Clinical Results
Many case studies and clinical trials have shown that modern occipitocervical fusion systems work effectively. These studies report the following facts.
-> Occipitocervical fusion with current tools shows a highly successful fusion rate at the occipitocervical junction.
-> A person’s neck is more stable and feels less pain after occipitocervical fusion surgery.
-> The risks of problems like implant failure or infection at the surgery site are low in occipitocervical fusion treatments.
-> Minimally invasive occipitocervical fusion has the same fusion rates as standard open surgery, but less blood is lost shorter hospital stays, and faster recovery.
-> Occipitocervical fusion is a good and long-lasting way to treat children with different spine conditions that were born with them or that they got later in life.
-> Long-term follow-up evaluations of occipitocervical fusion show that neurological function, pain relief, and functional skills continue to get better.
These results show that current occipitocervical systems are safe and work well to improve patient outcomes and reduce complications.
Surgeon Perspectives
From the surgeon’s perspective, the development of contemporary Occipitocervical Fusion Systems has simplified difficult surgeries’ performance, permitting perfect fixation and alignment.
The ability to personalize treatment and improve surgical planning has been made possible by the availability of customizable implants.
Surgeons have observed an increase in their confidence level in their ability to do successful fusions, and the shorter operating times have decreased the total strain placed on the healthcare system.
Patient Perspectives
For the benefit of patients, the development of occipitocervical fusion systems has been a step forward in the right direction.
There has been a discernible shift toward shorter periods of time needed for recovery, shorter lengths of stays in the hospital, and an overall improvement in post-operative quality of life.
Patients who previously faced extended periods of immobility and rehabilitation can now return to their everyday routines with much less difficulty than in the past.
In addition, the decrease in the likelihood of problems and the enhancement of the outcomes over the long term have contributed to a larger degree of trust in the Occipitocervical Fusion System surgical method.
Future Directions and Innovations
The future of the Occipitocervical Fusion System has a lot of potential to make things better for patients and change how problems of the upper cervical spine are treated.
-> Advanced 3D printing technology is used to make implants that fit each patient better and improve fusion results.
-> Biologically enhanced fusion materials are made by adding biological substances or growth factors to fusion materials to help bones fuse faster and more reliably.
-> Using high-tech guidance tools to make surgery more precise, improve screw placement, and lower the risk of problems.
-> An in-depth biomechanical study is done to learn more about the forces and stresses on the occipitocervical region. It helps improve the design and stability of implants.
-> Combining AI and ML algorithms to look at patient data, predict what will happen during surgery, and make the best care plans for each patient.
-> Encouraging medical institutions to work together on research and share data to speed up innovation and progress in occipitocervical fusion.
-> Using patient-reported outcomes and measures of quality of life to figure out how well occipitocervical fusion surgeries work in the long run.
-> Working with regulatory officials to speed up the approval process for new occipitocervical fusion technologies so that patients can use them as soon as possible.
Conclusion
The development of the occipitocervical fusion system is a huge step forward for spinal health care. Complex spinal conditions can now be treated in a manner that is safer, more dependable, and extremely effective as a result of ongoing innovation and developments in technology.
As the field keeps getting better, the future of occipitocervical fusion looks very promising. It could lead to better care for patients and better surgery. Because of these innovations, occipitocervical fusion is a great example of how new medical ideas can really change people’s lives.

